The Quest for a Diabetes Cure: Understanding Current Research and Future Possibilities
Understanding Diabetes: A Complex Disease
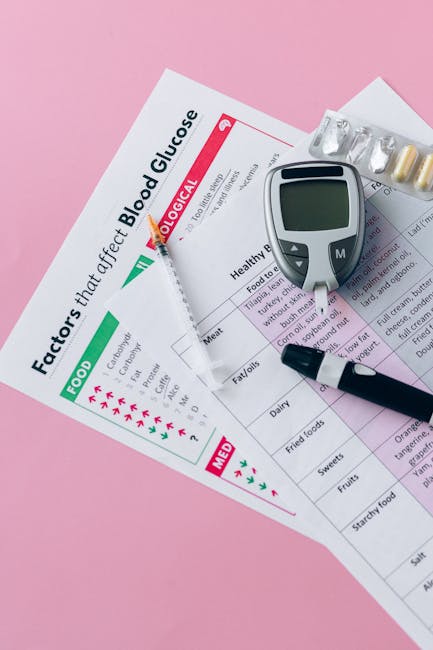
Diabetes, a chronic metabolic disorder, affects millions worldwide. Characterized by high blood sugar levels, it stems from the body’s inability to produce enough insulin (type 1) or effectively use the insulin it produces (type 2). This leads to a cascade of health problems, including heart disease, kidney failure, nerve damage, and blindness. While there’s no single ‘cure’ currently available, significant strides are being made in management and treatment, and research into a potential cure continues to advance.
Type 1 Diabetes: Autoimmune Assault
Type 1 diabetes is an autoimmune disease where the body’s immune system mistakenly attacks and destroys the insulin-producing beta cells in the pancreas. This leaves individuals entirely dependent on external insulin administration for survival. Research focuses heavily on:
- Immunotherapy: Strategies aimed at suppressing the autoimmune response and protecting remaining beta cells. This includes approaches like immune tolerance induction and the use of immunosuppressive drugs.
- Stem cell therapy: Replacing destroyed beta cells with new, healthy ones grown from stem cells. Significant challenges remain in efficiently generating functional beta cells and ensuring their long-term survival.
- Pancreatic islet transplantation: Transplanting healthy islet cells (clusters of cells containing beta cells) from a donor pancreas. While effective, it requires lifelong immunosuppressant medication and faces challenges related to donor organ availability.
Type 2 Diabetes: Lifestyle and Genetics Intertwined
Type 2 diabetes, far more prevalent, results from insulin resistance—the body’s cells don’t respond properly to insulin. Genetic predisposition plays a role, but lifestyle factors like obesity, physical inactivity, and poor diet significantly contribute. Research focuses on:
- Lifestyle interventions: Weight loss, regular exercise, and a healthy diet remain cornerstones of type 2 diabetes management. These changes can significantly improve insulin sensitivity and even lead to remission in some cases.
- Novel medications: Beyond traditional insulin and oral hypoglycemic agents, newer medications target various aspects of the disease, including GLP-1 receptor agonists, SGLT2 inhibitors, and DPP-4 inhibitors. These drugs enhance insulin secretion, improve insulin sensitivity, and increase glucose excretion.
- Gene therapy: Targeting genetic defects that contribute to insulin resistance and beta-cell dysfunction. This is a promising area, but still in its early stages of development.
- Bariatric surgery: Weight-loss surgery can dramatically improve insulin sensitivity and even lead to remission in some individuals with type 2 diabetes. However, it’s an invasive procedure with potential risks.
Promising Avenues of Research: The Path Towards a Cure
Regenerative Medicine: Growing New Beta Cells
Significant progress is being made in developing methods to generate functional beta cells from stem cells. This holds immense potential for treating both type 1 and type 2 diabetes by replacing damaged or deficient cells. Researchers are exploring different stem cell sources and refining differentiation protocols to improve the efficiency and functionality of the generated beta cells. Encapsulation techniques are also being investigated to protect transplanted cells from immune rejection.

Immunomodulation: Taming the Immune System
For type 1 diabetes, strategies to regulate the autoimmune response are crucial. Immunotherapy approaches aim to prevent the destruction of beta cells or even reverse the autoimmune attack. This involves the use of immune-suppressing drugs, antibodies that target specific immune cells, and novel approaches like immune tolerance induction. The goal is to achieve a state of immune equilibrium where the body no longer attacks its own beta cells.
Gene Editing: Precision Medicine
CRISPR-Cas9 and other gene-editing technologies offer exciting possibilities for correcting genetic defects that contribute to diabetes. Researchers are exploring the potential of gene editing to enhance insulin production, improve insulin sensitivity, or correct genetic mutations that lead to increased risk of diabetes. However, ethical considerations and potential off-target effects need careful consideration.
Artificial Pancreas: Mimicking Natural Function
The artificial pancreas, a closed-loop system combining an insulin pump with a continuous glucose monitor (CGM), is already revolutionizing diabetes management. This technology automatically adjusts insulin delivery based on real-time glucose levels, providing more precise and personalized control. Further research focuses on improving the accuracy, reliability, and ease of use of these systems.
Gut Microbiome: A Hidden Player
Emerging research highlights the role of the gut microbiome in diabetes development and progression. The composition and function of gut bacteria can influence insulin sensitivity, inflammation, and glucose metabolism. Studies are investigating the potential of manipulating the gut microbiome through diet, probiotics, or fecal microbiota transplantation to improve diabetes management.

Challenges and Ethical Considerations
The quest for a diabetes cure faces several significant challenges. These include:
- Complexity of the disease: Diabetes is a multifaceted disease with multiple contributing factors, making it difficult to develop a single, universally effective cure.
- Immune rejection: Transplantation approaches face challenges related to immune rejection of transplanted cells or organs.
- Long-term effects: The long-term safety and efficacy of new therapies need to be thoroughly evaluated.
- Cost and accessibility: New treatments may be expensive and potentially inaccessible to many individuals.
- Ethical considerations: Gene editing and other advanced technologies raise ethical concerns about safety, accessibility, and potential misuse.
Conclusion: Hope on the Horizon
While a complete cure for diabetes remains elusive, the research landscape is vibrant and promising. Significant progress is being made in understanding the underlying mechanisms of diabetes and developing innovative therapies. Advances in regenerative medicine, immunomodulation, gene editing, and other approaches offer hope for a future where diabetes can be effectively prevented, managed, or even cured. Continued research, collaboration, and commitment are crucial to realizing this vision and improving the lives of millions affected by this chronic disease.